GRC Alternatives
Feb 3, 2026
10 Radar Healthcare Alternatives: The Best Risk, Quality & Compliance Platform
Written by: Tanaka Chamisa
A guide for healthcare leaders evaluating risk, quality, and compliance software, what actually reduces admin, improves visibility, and scales governance.
Healthcare organisations operate in an environment of constant scrutiny, growing complexity, and rising expectations. Incidents must be reported and investigated quickly.
Policies must be kept up to date and evidenced. Training must be tracked. Audits must be ready at any moment, not just when an inspection is scheduled.
For many UK and international healthcare providers, Radar Healthcare has long been a familiar name in this space.
It’s a well-established platform used across NHS trusts, care providers, and healthcare organisations to support incident reporting, risk management, and quality improvement.
But as healthcare systems scale, digitise, and modernise, many teams are asking a more nuanced question:
Is our current governance system helping us operate better or simply helping us record what already happened?
In this article, we explore Radar Healthcare’s strengths, where organisations may start to feel constrained, and the best Radar Healthcare alternatives for providers looking to strengthen quality, risk, and compliance without adding administrative burden.
Understanding Radar Healthcare in Context
Radar Healthcare is a recognised name in UK healthcare governance largely because it aligns well with traditional quality, risk, and assurance structures.
Its strengths sit squarely within established governance models that prioritise formal reporting, documentation, and review.
Below is a deeper look at the areas Radar Healthcare is primarily known for, and what that means in practice for healthcare organisations.
Incident Reporting and Investigation
Radar Healthcare is widely used as a centralised incident reporting tool, allowing staff to log adverse events, near misses, and concerns in a structured way.
In practice, this means:
Standardised incident forms
Categorisation by severity, type, and service area
The ability to assign incidents for investigation and follow-up
Audit trails that support regulatory scrutiny
For many organisations, Radar has helped replace informal or fragmented incident reporting methods (e.g. emails, spreadsheets, paper forms) with a single, auditable system.
However, incident management within Radar often remains process-driven rather than outcome-driven. Incidents are captured and investigated, but:
Follow-up actions can become manual
Escalations may rely on people remembering to act
Cross-team visibility can be limited
Learning doesn’t always flow automatically into policy, training, or risk updates
As volumes increase, teams can find themselves managing the system rather than the underlying risk.
Risk Registers and Risk Management
Radar supports the creation and maintenance of risk registers, a core requirement for most healthcare providers.
This typically includes:
Defining risks and controls
Assigning owners
Reviewing likelihood and impact
Producing reports for governance committees
For organisations with established governance frameworks, this works well as a formal record of known risks.
The challenge arises when risk management becomes:
Retrospective rather than proactive
Decoupled from real operational activity
Updated periodically rather than continuously
Many teams report that risks are reviewed because they are scheduled, not because the system is surfacing new signals. This can create a gap between what is documented and what is actually happening on the ground.
Quality & Governance Workflows
Radar Healthcare is often positioned as a quality and governance platform, supporting:
Quality improvement initiatives
Governance reviews
Committee reporting
Assurance frameworks
This aligns strongly with traditional healthcare governance structures, particularly in the NHS and regulated care environments.
Where this works well:
Formal governance reporting
Structured assurance processes
Supporting compliance narratives
Where organisations can struggle:
Governance workflows often feel separate from day-to-day operations
Evidence is pulled together after the fact
Teams spend time preparing reports rather than acting on insights
Governance becomes something that happens to teams, not with them
As organisations grow or decentralise, this separation can reduce the perceived value of governance systems among frontline teams.
Supporting Compliance and Improvement Initiatives
Radar Healthcare plays an important role in helping organisations demonstrate compliance with regulatory expectations.
This includes:
Evidence for inspections
Documentation of actions taken
Structured responses to findings
Tracking improvement plans
For compliance-led organisations, this provides reassurance and structure.
However, compliance support in Radar often assumes:
Dedicated governance capacity
Manual coordination between systems
Human intervention to keep everything aligned
As regulatory pressure increases and resources remain constrained, organisations start asking whether their compliance system is reducing risk or simply recording it.
Why Consider a Radar Healthcare Alternative?
Most organisations do not replace a solution like Radar Healthcare because it “doesn’t work”. They explore alternatives because their operating reality has changed.
Below are the most common reasons healthcare providers may begin evaluating other options.
Governance Beyond Incident Reporting
Many healthcare organisations reach a point where incident reporting alone is no longer enough.
They want governance systems that:
Connect incidents to risks automatically
Trigger reviews, training, or policy updates without manual coordination
Surface patterns early, not months later
Provide leadership with a live view of organisational health
In these environments, governance is no longer a collection of tools; it’s a system that must operate continuously.
When governance platforms focus primarily on capturing events rather than orchestrating responses, teams start to feel the limitations.
Reducing Manual Admin and Chasing
One of the most common pain points driving change is administrative overhead.
Healthcare teams often report:
Manually following up on actions
Chasing acknowledgements or updates
Copying data between systems
Preparing reports that duplicate existing information
Over time, this creates:
Burnout among governance and quality teams
Lower engagement from frontline staff
Delays in resolving issues
Increased risk despite “good” reporting
Organisations begin to look for platforms that enforce timelines, escalate automatically, and reduce reliance on memory and goodwill.
Consistency Across Sites and Teams
As healthcare providers expand across regions, services, or care settings, process consistency becomes critical.
Common challenges include:
Different teams handling similar incidents differently
Inconsistent thresholds for escalation
Variation in documentation quality
Difficulty comparing performance across sites
Traditional governance tools often allow flexibility, but at scale, this can become fragmentation.
Alternatives are often explored when leadership wants:
Standardised workflows
Clear ownership everywhere
Local autonomy within global guardrails
Confidence that “the same thing means the same thing” across the organisation
Trusted, Actionable Data for Leadership
Finally, many organisations begin looking elsewhere when data stops being trusted.
This happens when:
Reports are static and backwards-looking
Data is spread across multiple systems
Metrics are debated instead of being acted upon
Leaders lack confidence in what they’re seeing
Modern leadership teams want:
Real-time insight
Clear trends
Evidence they can stand behind
Early warning signals, not post-mortems
When governance data requires heavy interpretation or reconciliation, it loses strategic value, and organisations start looking for platforms designed around decision-making, not just documentation.
Best Radar Healthcare Alternatives for Risk, Quality & Compliance
The platforms below are commonly evaluated alongside Radar Healthcare by organisations looking to strengthen governance, reduce manual admin, and gain better visibility across quality, risk, and compliance.
Each serves a different type of organisation and maturity level.
1. Safe Workplace
Overview
Safe Workplace is a governance, risk, and compliance platform designed for organisations operating at scale. In healthcare, it focuses on turning everyday operational activity into clear oversight, evidence, and early intervention without increasing administrative load.
Unlike traditional governance tools, Safe Workplace is built around connected systems, automation, and real-time visibility. Brands using Safe Workplace have achieved up to 50% faster incident resolution.
Who It’s For
Hospitals and health systems
Care groups and social care providers
Digital-first healthcare organisations
Large, multi-site or regulated healthcare environments
Core Strengths
Strong focus on outcomes, not just reporting
Automation that reduces manual follow-up
Consistent workflows across teams and locations
Leadership-ready reporting and BI
Key Modules & Capabilities
Incident & Case Management
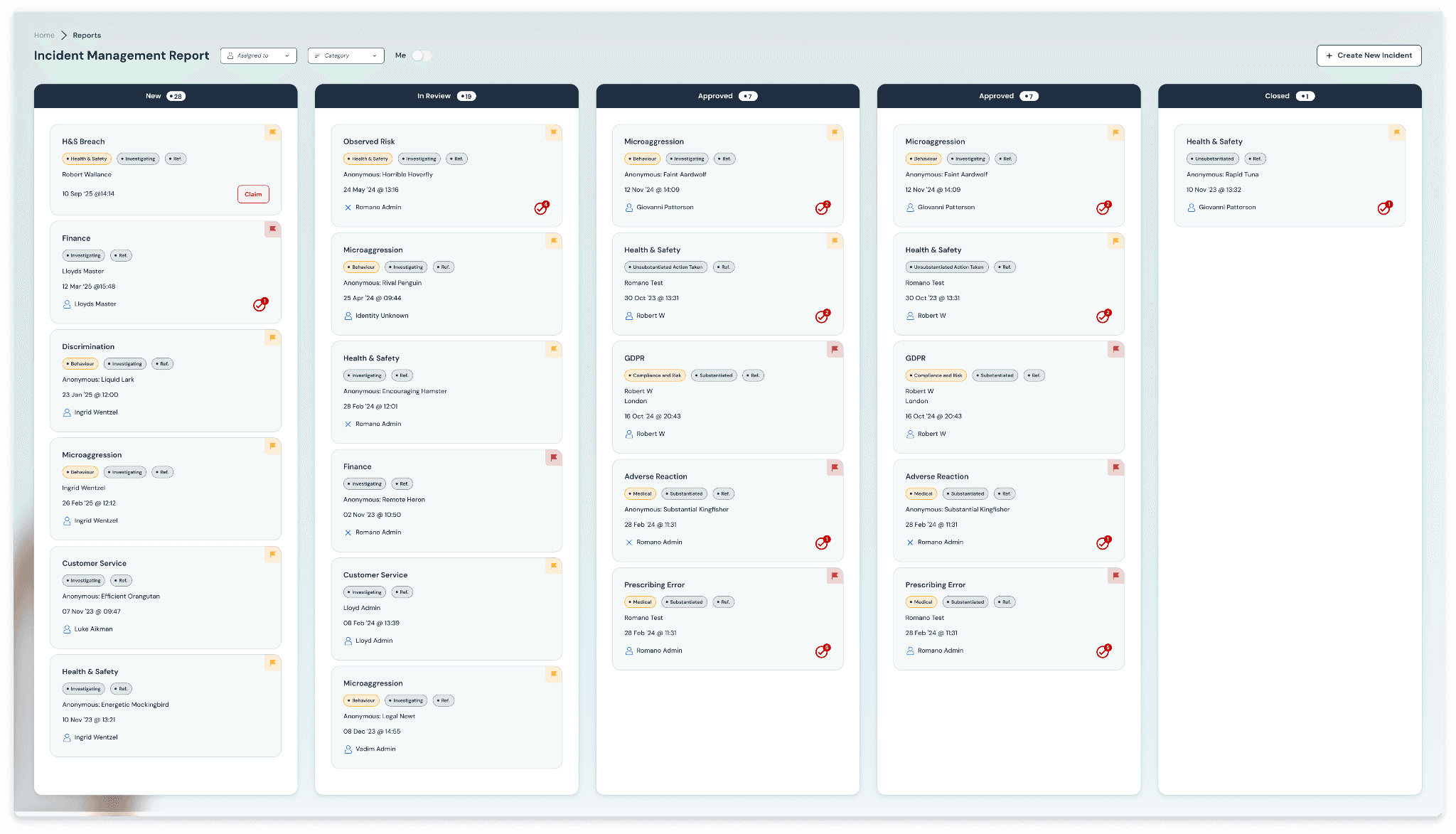
Capture, route, escalate, and resolve incidents with:
Automated workflows
Clear ownership and accountability
Consistent handling across departments
Policy Management

Centralised policies
Version control and acknowledgements
Evidence of understanding, not just storage
Training Management
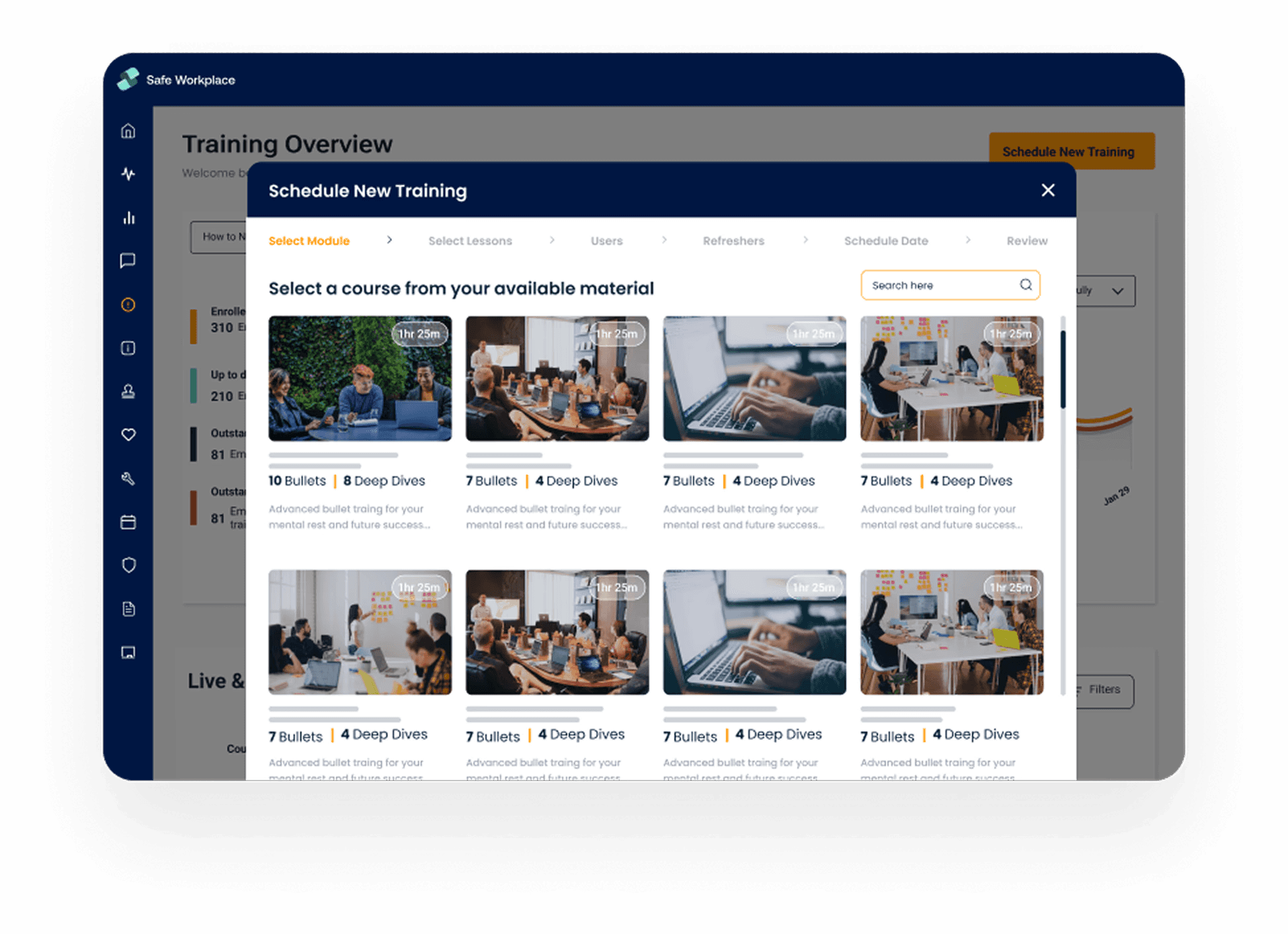
Track mandatory and role-based training
Link training directly to incidents, audits, and risks
Identify gaps before they become findings
Audit & Assurance
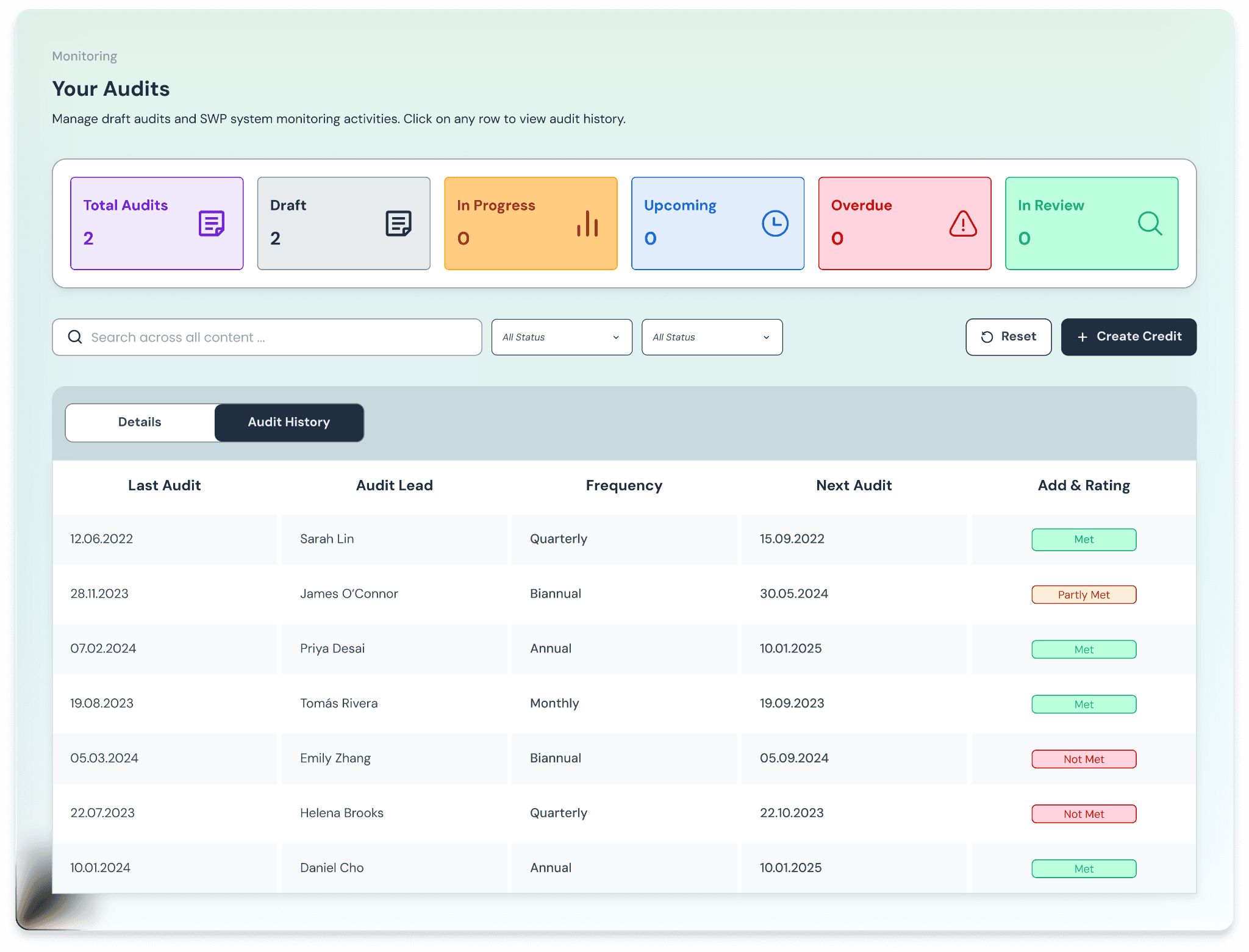
Continuous audit readiness
Evidence collected automatically through day-to-day activity
Reduced inspection stress
Risk Management
Live risk registers
Controls linked to real operational data
Visibility into emerging issues, not just historical ones
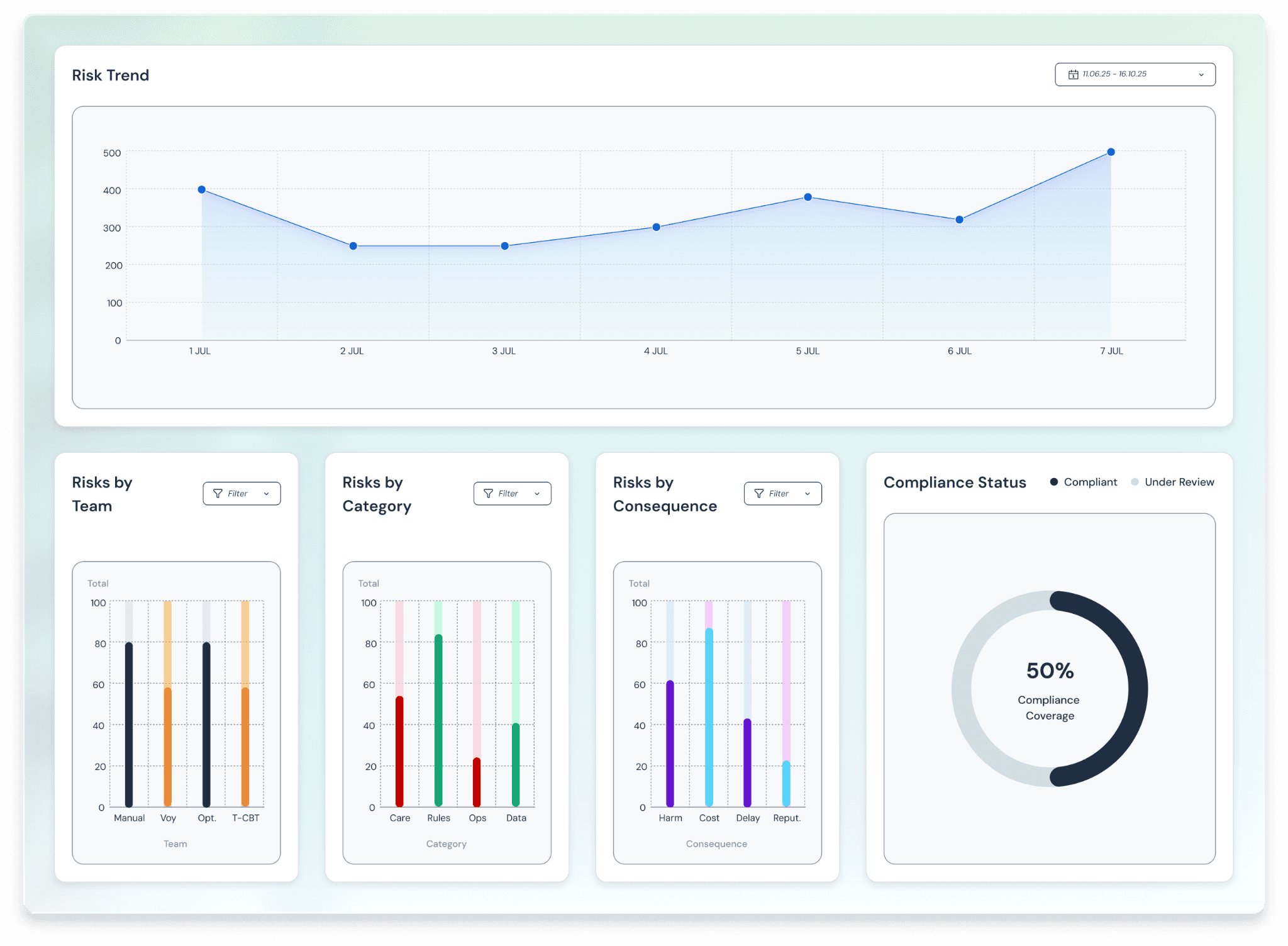
Reporting & Business Intelligence
One source of truth for governance data
Executive-level dashboards
Trusted data leaders can act on
Pros
Designed for scale and complexity
Reduces admin and chasing significantly
Integrates with HR, communication, and operational tools
Strong fit for organisations seeking modern governance
Considerations
Less suitable for very small or single-site providers with minimal governance needs
Requires buy-in to a systems-based approach
Pricing
Pricing is typically modular and organisation-specific, based on:
Size
Number of sites
Required modules
Level of customisation
2. Ideagen
Overview
Ideagen provides a broad suite of governance, risk, and compliance solutions used across healthcare, aviation, finance, and other regulated sectors. In healthcare, Ideagen is often positioned as an enterprise-grade platform supporting audits, risk registers, document control, and compliance reporting.
Its strength lies in formal governance and assurance structures, particularly where organisations need to demonstrate alignment with regulatory frameworks and standards.
Who it’s best for
NHS trusts and large healthcare providers
Highly regulated public-sector organisations
Enterprises with formal governance and audit teams
Pros and cons
Pros
Strong audit and compliance capabilities
Well-suited to formal governance environments
Established presence in regulated sectors
Cons
Can feel process-heavy for frontline teams
Limited automation for day-to-day operational workflows
Governance often remains detached from real-time activity
3. Datix (RLDatix)
Overview
Datix is widely known in healthcare, particularly in the NHS, for its focus on patient safety, incident reporting, and risk management. It has a strong reputation in clinical safety and adverse event reporting.
Datix excels in capturing incidents and supporting safety analysis, but is often perceived as complex and heavily configured, especially outside large institutional settings.
Who it’s best for
NHS trusts and large hospital systems
Patient safety and clinical governance teams
Organisations with established Datix expertise
Pros and cons
Pros
Strong clinical incident reporting
Trusted brand in patient safety
Deep functionality for safety analysis
Cons
Complex configuration and administration
Limited flexibility for non-clinical governance use cases
Slower to adapt to modern, distributed operations
4. Navex
Overview
Navex is a global Governance, Risk & Compliance (GRC) platform best known for ethics, compliance, and whistleblowing solutions. It is widely used across large enterprises to manage regulatory compliance, third-party risk, policy acknowledgement, and speak-up programmes.
In healthcare, Navex is typically adopted for corporate compliance and ethics functions, rather than operational quality or clinical governance.
Who it’s best for
Large enterprises across industries
Corporate compliance and legal teams
Organisations with strong ethics & whistleblowing requirements
Pros and cons
Pros
Market leader in whistleblowing and ethics reporting
Strong policy management and compliance frameworks
Well-established global brand
Cons
Less suited to operational healthcare workflows
Limited depth in the incident lifecycle and quality improvement
Governance often sits outside day-to-day operations
5. MasterControl Quality Excellence
Overview
MasterControl is a leading enterprise QMS platform, particularly strong in life sciences and regulated manufacturing. Its Quality Excellence suite offers deep document control, CAPA, audits, and training management.
While powerful, MasterControl is designed for validation-heavy environments and can feel overly rigid for operational healthcare governance.
Who it’s best for
Medical device manufacturers
Pharmaceutical and biotech companies
Highly regulated manufacturing organisations
Pros and cons
Pros
Industry-leading document control
Strong CAPA and validation capabilities
Excellent regulatory alignment
Cons
Heavy implementation effort
Less suited to frontline healthcare workflows
High learning curve for non-QA users
6. Qualio
Overview
Qualio is a modern, cloud-based QMS designed to simplify compliance for growing regulated organisations. It focuses on ease of use, fast deployment, and core quality processes.
Qualio is often chosen by smaller or earlier-stage organisations rather than complex healthcare systems.
Who it’s best for
Medical device and life sciences startups
Small to mid-sized regulated organisations
Teams early in their compliance journey
Pros and cons
Pros
Clean, user-friendly interface
Faster implementation than enterprise QMS tools
Good document and training management
Cons
Limited depth in incident and risk management
Not designed for large, distributed healthcare operations
Less flexibility at enterprise scale
7. ETQ Reliance
Overview
ETQ Reliance is a modular enterprise QMS platform used across manufacturing, life sciences, and regulated industries. It offers extensive configurability across quality, compliance, and audit processes.
Its flexibility comes at the cost of complexity, requiring significant internal ownership.
Who it’s best for
Large regulated enterprises
Manufacturing and life sciences organisations
Dedicated quality and compliance teams
Pros and cons
Pros
Highly configurable
Broad quality and compliance coverage
Strong enterprise reporting
Cons
Complex setup and ongoing management
Heavy administrative overhead
Less intuitive for frontline healthcare teams
8. SafetyCulture
Overview
SafetyCulture is best known for iAuditor, a mobile-first inspection and checklist platform. It’s widely used for operational safety and compliance checks across many industries.
While excellent for capturing frontline activity, it lacks depth in governance, risk lifecycle management, and healthcare-specific compliance.
Who it’s best for
Operational safety teams
Construction, facilities, and retail
Organisations focused on inspections
Pros and cons
Pros
Extremely easy to use
Strong mobile experience
Fast deployment
Cons
Limited incident and risk lifecycle management
Not healthcare-specific
Shallow governance capabilities
9. Cority
Overview
Cority is a global EHS and sustainability platform used by large enterprises. It excels in occupational health, safety, and environmental compliance.
In healthcare contexts, Cority is typically used for EHS rather than broader quality and governance needs.
Who it’s best for
Large industrial and infrastructure organisations
Global EHS programmes
Occupational health teams
Pros and cons
Pros
Strong EHS and occupational health functionality
Scales globally
Advanced analytics
Cons
Less focused on healthcare governance
Long implementation cycles
Complex platform
10. GoAudits
Overview
GoAudits is a mobile audit and inspection platform focused on operational compliance and site-level visibility. It prioritises speed and simplicity over deep governance.
Who it’s best for
Multi-site retail and hospitality
Facilities and operations teams
Operational audit programmes
Pros and cons
Pros
Fast deployment
Simple audit workflows
Good site-level visibility
Cons
Limited risk and incident management
Not designed for healthcare governance
Shallow reporting for leadership
Radar Healthcare Alternatives Comparison
Platform | Best For | Core Strength |
|---|---|---|
Radar Healthcare | Traditional healthcare governance | Incident & risk reporting |
Safe Workplace | Complex, multi-site healthcare | Reporting, connected governance & automation |
Ideagen | Formal governance environments | Audit & compliance structure |
Datix (RLDatix) | NHS patient safety | Clinical incident depth |
Navex | Corporate compliance & ethics | Whistleblowing & policy compliance |
MasterControl | Life sciences & manufacturing | Deep QMS & validation |
Qualio | Early-stage regulated orgs | Simple, modern QMS |
ETQ Reliance | Large regulated enterprises | Configurable enterprise QMS |
SafetyCulture | Frontline inspections | Mobile audits & checklists |
Cority | Global EHS programmes | EHS & occupational health |
GoAudits | Operational audits | Fast site audits |
What to Look for in Risk, Quality & Compliance Software
Choosing a risk, quality, and compliance platform is rarely about features alone.
Most healthcare organisations already have tools. The real question is whether those tools are helping teams operate better or adding friction.
Here are the criteria that matter most once organisations move beyond basic reporting.
1. Does the System Reduce Work or Just Move It Around?
Many governance platforms promise structure, but in practice simply shift the workload from one place to another.
Instead of chasing emails, teams chase dashboards. Instead of spreadsheets, they manage workflows. Instead of preparing reports manually, they prepare the system for reporting.
Over time, this creates a familiar pattern: the system is technically “in place”, but adoption depends on a small group of people doing a lot of invisible work to keep it running.
Strong governance software should do the opposite. It should:
Remove manual follow-ups through automation
Enforce timelines and ownership without human chasing
Reduce duplication rather than formalise it
If compliance relies on goodwill and effort, it won’t scale.
2. Can Leaders See What’s Actually Happening?
Most healthcare leaders don’t lack data. They lack confidence in the data.
When insight is delayed, filtered, or heavily summarised, it becomes hard to answer basic questions:
Where are issues increasing?
What keeps repeating?
Which risks are actually under control?
Dashboards should not exist solely for governance meetings. They should reflect live operational reality, built from day-to-day activity rather than retrospectively assembled reports.
The test is simple:
Can leadership act on what they see without first questioning its accuracy?
3. Are Processes Truly Consistent?
Many organisations believe their processes are consistent because they are documented.
In reality:
Similar incidents are handled differently by different teams
Escalation thresholds vary by site or manager
Follow-up actions depend on individual judgement
This isn’t a failure of people. It’s a failure of systems.
Effective governance software doesn’t just describe the process — it enforces it:
The same steps, everywhere
Clear ownership at each stage
Predictable escalation when something stalls
Consistency is not about control. It’s about fairness, safety, and reliability at scale.
4. Is Governance Continuous?
A common sign that a platform is no longer fit for purpose is remembering it only when an inspection is due.
In episodic governance models:
Evidence is gathered in bursts
Teams scramble to close gaps
Compliance feels reactive and stressful
Modern healthcare environments require something different:
governance that operates quietly in the background, all the time.
That means:
Evidence is created as work happens
Risks surface early, not at review points
Readiness becomes a by-product of normal operations
If a system only feels useful during audit season, it’s not doing enough.
5. Does the Platform Connect to Reality or Sit Beside It?
Healthcare organisations already run on multiple systems: HR, clinical, scheduling, communication, and more.
The question isn’t whether a governance platform can replace these systems — it shouldn’t.
The question is whether it can connect them meaningfully.
Strong platforms:
Pull in context from existing tools
Push actions and notifications where teams already work
Reduce context-switching and double entry
Weak platforms operate in isolation, forcing teams to bridge the gaps manually.
Governance doesn’t need another silo. It needs a connective layer.
The Best Radar Healthcare Alternative for You
Radar Healthcare remains a respected and widely used platform. For many organisations, it has played an important role in establishing governance foundations.
However, healthcare organisations facing scale, complexity, and growing operational pressure often find they need more than reporting, they need clarity, consistency, and confidence in real time.
That’s where modern alternatives like Safe Workplace enter the conversation.
Want to see how Safe Workplace compares in practice?
Book a demo to explore how governance can move from administration to advantage.


